There comes a moment when even small joys stop feeling like joy. The coffee you once savored tastes flat. The song that once made you sing now feels like background noise. The world, somehow, feels a size too tight.
You tell yourself you’re just tired, overworked, or going through “a phase.” But sometimes, it’s more than that. Sometimes, your body is trying to whisper through your mind that something deeper is off-balance.
This dimming of interest and energy, the quiet erosion of motivation and pleasure, is one of the earliest signs of depression, a condition that affects more than 300 million people globally, according to the World Health Organization. And while depression is often framed purely as an emotional or psychological disorder, science is uncovering a deeper truth: your brain’s chemistry, and even the nutrients fueling it, can dramatically influence how you feel.
Clinically, depression is defined not just by sadness but by anhedonia, the inability to feel pleasure. To qualify as a depressive episode, symptoms must persist for at least two weeks and include changes in sleep, appetite, fatigue, low concentration, or feelings of worthlessness.
These symptoms aren’t signs of weakness. They are signals of imbalance, chemical, emotional, and often nutritional. A lack of certain nutrients doesn’t cause depression outright, but emerging research shows that deficiencies can worsen its depth or blunt recovery.
The good news? Correcting those imbalances, precisely and scientifically, can help tilt the scale toward healing.
Among all nutrients studied in mood science, L-methylfolate, the active form of vitamin B9, has one of the most compelling backstories. Folate acts as a biochemical architect, building and balancing neurotransmitters like serotonin, dopamine, and norepinephrine, the very chemicals that define our emotional weather.
But here’s the twist: not everyone processes folate efficiently. Genetic variations in the MTHFR gene can limit your body’s ability to convert standard folic acid into its active form. That means even if your diet is full of greens, your brain might still be short on the raw material it needs to make “happy chemicals.”
A 2023 clinical review published in Psychiatrist.com found that supplementing with L-methylfolate can improve outcomes in patients who respond only partially to antidepressants, especially those with higher inflammation or BMI. It’s not a magic bullet, but it’s no longer fringe science either. Under medical supervision, L-methylfolate has become a clinically reasonable adjunct to depression treatment, helping antidepressants work more efficiently in select patients.
In short your therapy and medication may be doing their job, but your biochemistry might need a little extra help building the foundation.
If folate is architecture, omega-3 fatty acids are the building materials. Specifically, EPA and DHA, the marine-derived fats found in fish oil, are essential for keeping your brain cells flexible and your mood stable. They’re anti-inflammatory, neuroprotective, and crucial for proper neurotransmission.
For years, studies have hinted that higher omega-3 intake is linked to lower rates of depression. But what does the latest evidence say?
A 2024 meta-analysis found that omega-3 supplements, particularly those high in EPA, offered modest but meaningful improvements when used alongside standard treatments. The catch? The certainty of the evidence was rated as “very low.” Translation: omega-3s are safe, promising, and worth trying for some, but not a guaranteed fix.
If you and your doctor decide to try them, look for formulations that deliver at least 1-2 grams of EPA daily, and track your mood over 6-8 weeks. The effect is subtle, a smoothing of edges rather than a dramatic turnaround, but it’s real enough to matter.
There’s a reason winter blues and vitamin D deficiency often go hand in hand. Vitamin D isn’t just for bones, it has receptors scattered throughout the brain, influencing the genes that regulate mood.
A 2025 meta-analysis in Frontiers in Psychiatry confirmed that supplementing with vitamin D₃ can reduce depressive symptoms, particularly in those with low baseline levels. Researchers described it as a “short-term mood elevator” that still needs longer-term trials for clarity.
In practice, this means vitamin D is best approached as a test-and-treat nutrient. Don’t supplement blindly. Get a blood test, replete under guidance, and monitor not just your lab numbers but your mental clarity and energy. Sometimes, the smallest correction, like restoring vitamin D to optimal levels, can shift the emotional tone of your day.
When your motivation nosedives, it’s tempting to reach for supplements that promise to “boost dopamine.” One of the most popular is L-tyrosine, the amino acid that serves as a raw material for dopamine and norepinephrine.
On paper, it makes perfect sense. In reality, science doesn’t back it up. A randomized, double-blind study comparing tyrosine with imipramine (a standard antidepressant) found no antidepressant effect for tyrosine over four weeks.
The verdict? Tyrosine can sharpen focus and cognition under short-term stress (like sleep deprivation), but it doesn’t treat depression. Using it as a mood enhancer without guidance can even be risky for people with thyroid conditions or those on certain medications.
It’s a good reminder that not every “mood booster” on your feed is backed by real evidence.
The internet often buzzes with talk of “activated B-vitamins” and “biohacking your mood,” but the real key is personalization. Not everyone needs methylated forms of vitamins. What everyone does need is testing and targeting.
A simple set of labs, checking vitamin D, B12, folate, iron, and thyroid levels, can guide a plan that’s both effective and safe. Deficiencies, once corrected, often lead to noticeable improvements in mood, focus, and energy. But flooding the body with megadoses rarely helps and can sometimes harm.
As psychiatrist and nutrition researcher Dr. Drew Ramsey puts it, “The brain doesn’t heal with more; it heals with balance.”
Even the most sophisticated supplement plan fails without the basics. Exercise, consistent sleep, nutrient-rich meals, and social contact are not “extras” ; they’re medicine.
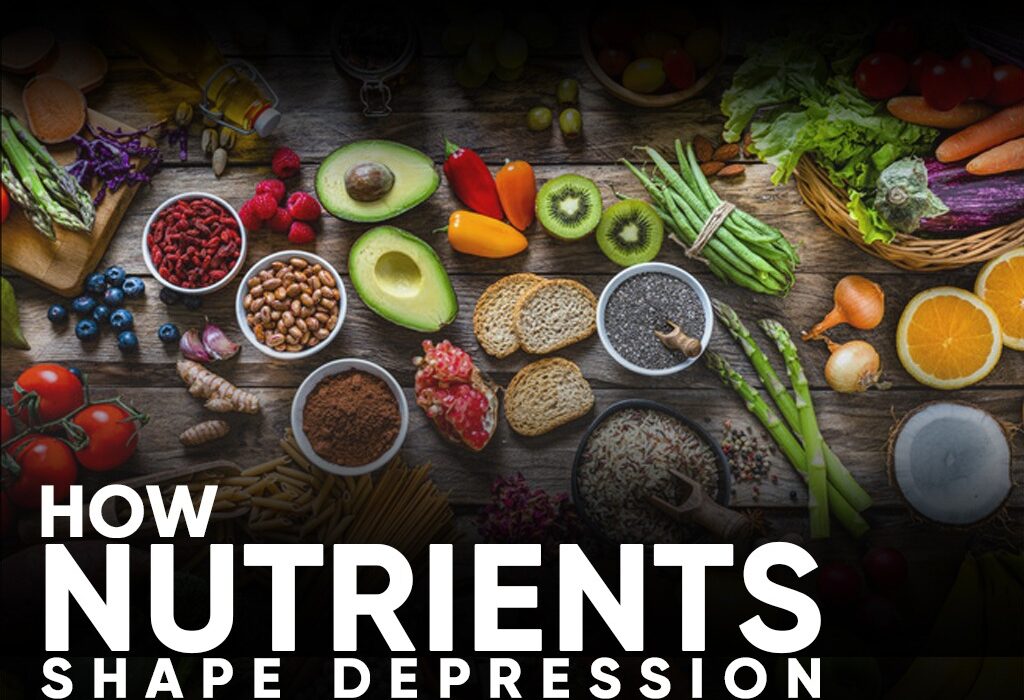
A Mediterranean-style diet, rich in olive oil, fish, legumes, fruits, and vegetables, has been shown in multiple trials to lower depression risk by up to 30%. Regular movement releases endorphins that rival antidepressants in effect size. Structured social contact, even when it feels impossible, can gently pull you back into life.
These aren’t side notes, they’re the pillars. They provide the scaffolding that therapy, medication, and nutrients can climb.
Here’s what the evidence really says:
● L-methylfolate helps some partial responders to antidepressants.
● Omega-3s, especially EPA, may ease depressive symptoms modestly.
● Vitamin D can brighten mood when deficiency exists.
● Tyrosine doesn’t replace treatment.
● And no supplement substitutes for clinical care.
Healing from depression is not about chasing superfoods or magic pills, it’s about restoring harmony between body and mind.
So if you’ve been feeling like the world has lost its color, start by listening, to your body, your doctor, your own quiet instincts. Get tested, get guided, and rebuild from within.
Because sometimes, the way back to yourself isn’t through willpower or wishful thinking, it’s through nourishment